Despite the availability of numerous diagnostic tools, dental practitioners continue to face challenges when it comes to determining whether to perform third-molar extractions.
For example, researchers from the University of Santiago de Compostela recently evaluated the value of panoramic radiographs in predicting lower third-molar extraction difficulty and technique and the influence of practitioner experience on predictive ability (Oral Medicine, Oral Pathology and Oral Surgery, June 1, 2010).
Fourteen dental practitioners with varying levels of experience evaluated the difficulty of lower third-molar extraction in a group of patients using a 100-mm visual analog scale (VAS) and a modified version of a surgical difficulty scale. The results were then compared to postoperative scores calculated using the same scale.
“The most common cause of fracture is exerting too much force.”
— Jay Friedman, D.D.S., M.P.H.
A tendency to underestimate the difficulty of procedures that was more pronounced in observers with greater experience levels was observed. The researchers also found a low level of agreement between preoperative and postoperative evaluations using the surgical difficulty scale, as well as an association between difficulty assessed preoperatively using the VAS and difficulty assessed postoperatively using the surgical difficulty scale.
"The use of panoramic radiographs does not allow practitioners to accurately predict lower third-molar extraction difficulty and technique, regardless of their level of experience," they concluded.
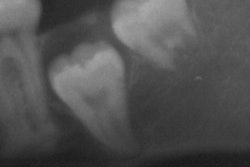
Another recent study showcased the risk of inferior alveolar neurovascular bundle (IANB) injury following third-molar removal, noting that IANB is one of the most common complications of third-molar removal and that "accurate preoperative radiographic assessment of surgical difficulty is necessary to correctly plan the removal of impacted third molars and to estimate the risk of IANB injury" (Journal of Craniofacial Surgery, July 2, 2010).
"Preoperative knowledge of the exact location of the third-molar roots in relation to the mandibular canal is mandatory," wrote researchers from the University of Turin. "A direct contact between the tooth and neurovascular bundle is suggested by a radiotransparent band across the roots of the impacted third molar on panoramic radiographs."
Cone-beam CT and finite element analysis
"For mandibular third molars, if the tooth lies above the mandibular canal without superimposition on the canal, a panoramic radiograph is likely sufficient," said Allan Farman, B.D.S., M.B.A., Ph.D., D.Sc., a professor of radiology and imaging science at the University of Louisville in Kentucky and president of the American Academy of Oral and Maxillofacial Radiology.
But 2D panoramic radiographs are not optimal when the root of the third molar is superimposed on the canal, Dr. Farman noted. "In this situation, well-collimated, relatively low-dose cone-beam CT provides better information for the clinician and the opportunity of better informed consent from the patient."
While cone-beam CT does not obviate all potential complications, "it does remove the blindfold from the eyes of the operator regarding association between canal and tooth root," he added.
Researchers from the University of Toronto and Semmelweis University are hoping to further improve the use of cone-beam CT for presurgically assessing third molars using finite element analysis (FEA). In a study published in the Journal of the Canadian Dental Association (JCDA, June 16, 2010), they analyzed the effects of removing various amounts of bone around an impacted mandibular third molar in order to predict the possibility of fracture due to excessive force.
"The purposes of this study were to build a detailed high-quality model of a human mandible with impacted third molars, to use the model to analyze the effects of removing various amounts of bone, and ultimately to simulate the different stages of bone removal and their impact on mandibular loading," the researchers wrote. "It was hoped that this would allow prediction of the risk of iatrogenic fracture of the mandible, as a means to help dentists to identify such risks preoperatively."
A panoramic radiograph and cone-beam CT scans of a 20-year-old woman with impacted third molars were retrieved from the database of the authors' clinic at Semmelweis. Data from the cone-beam CT scans were used to build 3D, patient-specific models of the mandible using FEA.
"Removal of a mandibular third molar may, in certain situations, weaken the mandible," the authors wrote. "The FEA models developed in this study showed that the external oblique ridge on each side was the location where stress was concentrated. Given the high mechanical stress associated with normal loading on the external oblique ridge, there is a possibility that the mandible will fracture during or after the procedure if large quantities of bone are removed."
With additional refinements and simplification, they added, the FEA method presented in this report could evolve into a more user-friendly modality for dentistry that could be used in the preoperative analysis of various surgical sites. "The results of FEA could then be used to predict the risk of iatrogenic fracture, thus providing dentists with more information to help in case selection and management of risk," they concluded.
Further development needed
But Dr. Farman cautions that FEA at present is not yet "clinic-friendly."
"I know of no ready-packaged, easy-to use, and sufficiently quick finite element analysis program that is available widely to practitioners," Dr. Farman said. "Hence, while this might provide excellent information in an academic center for a paper, thesis, or dissertation, its practicality would probably need to be developed for the 'real world' of practice."
Jay Friedman, D.D.S., M.P.H., who has written extensively on the issue of third-molar extractions, felt the study authors should have used a different case to illustrate the potential of FEA. While fractures may occur during third-molar surgery -- usually in the mandible at the angle of the jaw -- it would be "quite uncommon" in the removal of the lower teeth illustrated in the JCDA study, Dr. Friedman added.
"The authors could have used a better illustration with third molars deeply imbedded, at a 45° mesio-angulation, or horizontal, where bone needs to be removed," he said. "The most common cause of fracture is exerting too much force with an elevator because not enough bone was removed first, and/or the tooth was not properly sectioned. And because the extractions become so routine and easy for an experienced operator, he risks becoming cavalier about it and inadvertently exerts excessive force."
Copyright © 2010 DrBicuspid.com