As if the current global health crisis weren't stressful enough, consumer media, from the New York Times to the limericks on NPR's "Wait, Wait ... Don't Tell Me," recently reported that the anxiety of COVID-19 and the resulting quarantines has led to a rise of bruxism and fractured teeth.
While this is certainly possible -- who hasn't found themselves clenching their jaw over the past six months -- as an oral and maxillofacial radiologist, my thought is, "Yes, that makes sense -- but what else?" Through cone-beam computed tomography (CBCT) scan interpretation, I'm trained to look at each anatomical structure as if it were the culprit. Pandemic-induced stress may have caused a fracture, but what other issues lie beneath the surface?
Sometimes, the patient just needs a crown repaired -- and Dr. David Rice, clinical editor for DrBicuspid.com, has already shared how to safely and quickly treat patients -- but sometimes 3D imaging could reveal more. The affordability, ease-of-use, and compact size of today's multimodality CBCT systems, like a CS 8100 3D Evo Edition or CS 8200 3D (Carestream Dental), mean more general practitioners (GPs) are wanting to dig deeper with 3D on tricky cases.
General practitioners who are new to CBCT most often ask me the following: "When should I use 3D imaging?" and "When would a CBCT scan add value to my diagnosis?" Let's take the recent rise in bruxism and tooth fractures as an example.
Should you take a 3D scan for a cracked tooth? To determine when a CBCT scan might be beneficial, ask these questions:
- Are my clinical findings inconclusive?
- Can a 3D view affect my treatment plan?
- Will it help me localize the pathology?
If the answer to any of these questions is yes, a CBCT scan may be helpful. There are also standard clinical situations in which CBCT has been proved to be highly beneficial, several of which feature bruxism and fractures as symptoms.
 All images courtesy of Dr. Lea Al Matny.
All images courtesy of Dr. Lea Al Matny.TMJ issues
A low-dose 3D scan can be beneficial for evaluating the temporomandibular joint (TMJ), which is often affected by clenching and grinding, by providing a clear image of the condyles. With CBCT, a doctor can assess the volume and position of the condyle, determine the presence of asymmetry between right and left, evaluate the relationship between condyle and mandibular fossa, and detect changes that might suggest degenerative disease such as flattening, sclerosis, osteophyte formation, and erosion.
Vertical root fractures
In 2016, the American Academy of Oral and Maxillofacial Radiology (AAOMR) released a comprehensive update to the use of CBCT in endodontics, a joint statement with the American Association of Endodontists (AAE). Of the 12 recommendations for when limited fields-of-view (FOV) CBCT "should be considered the imaging modality of choice," 10 recommend that CBCT be used over intraoral radiography. In fact, the sixth recommendation states, "Limited FOV CBCT should be considered the imaging modality of choice if clinical examination and 2D intraoral radiography are inconclusive in the detection of vertical root fracture."
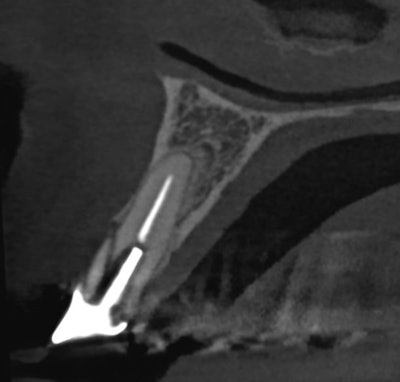
Fractures are typically caused by bone loss patterns around the root, meaning there's usually much more at play than what we can see during a clinical exam. When compared to a bitewing or panoramic, a 3D scan is significantly more successful at visualizing fractures, especially when combined with a focused field-of-view.
Occlusal trauma and periapical pathology
Radiographically, there are various signs that accompany occlusal trauma, such as widening of the periodontal ligament, thickening of the lamina dura, root resorption, hypercementosis, or periodontal bone loss. The forces exerted on teeth are applied to the occlusal surface, and, consequently, the root surfaces reflect these forces in terms of direction, size, frequency, and regularity. Occlusion trauma can also extend its effect from the level of the teeth to the level of temporomandibular structures.
Some reports also indicate that periapical pathology can be an underlying result of occlusal trauma. A 3D scan helps us identify the area of interest and localize the extent of pathosis and effect on surrounding anatomical structures. We can also determine a differential diagnosis and prognosis depending on radiographic behavior of the entity.
With COVID-19 having everyone reevaluating how to effectively fill schedules and manage cashflow, all while practicing safely, a 3D scan -- when used with guidance from the AAOMR and following the selection criteria provided by the ADA -- could provide a comprehensive view of the patient's dentition.
Does that mean you should take a 3D scan of every patient complaining of tight jaws and cracked teeth? No, a 3D scan should be a diagnostic tool complementary to a clinical exam. However, if you've properly followed through on your exams and have answered the questions above, then a 3D scan could ultimately save your patients and your practice time and money in the long run. Getting to the root of the problem right away and being able to start treatment planning immediately will keep patients from having to return over and over with the same pain.
So, unclench your jaw, take a deep breath, and ask yourself if a 3D scan could add value to your diagnosis and save you and your patients a lot of stress.
Dr. Lea Al Matny is a licensed oral and maxillofacial radiologist at SeeThru Reports and clinical education expert at Carestream Dental. She attended the University of Texas Health San Antonio (UTHSA) where she received both a certificate in oral and maxillofacial radiology and a master's degree in dental science. She is a reviewer for Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology and is actively involved in multiple committees at the American Academy of Oral and Maxillofacial Radiology.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.