Weeks after the placement of clear aligners, a woman had transient apical breakdown, a sequelae of dental trauma, that may have led to a purplish discoloration in a tooth that didn't respond to pulp tests, according to a case report that was published on February 18 in the Australian Endodontic Journal.
The woman's tooth returned to its original shade and responded to sensitivity tests a few months after her orthodontic treatment was suspended, wrote the author, Zufeng Zhu, MS, of the department of stomatology at Xiaoshan Traditional Chinese Medical Hospital in China.
"We here report a TAB (transient apical breakdown) case induced by orthodontic force whose maxillary right central incisor displayed crown discoloration and responded negatively to pulp sensitivity tests during clear aligner therapy," Zhu wrote.
A 24-year-old woman with diastema
The woman, who underwent orthodontic treatment 10 years earlier, visited the orthodontist due to a gap between her upper central incisors. Before orthodontic treatment was initiated, the clinician determined her incisors were vital and intact without caries or restorations.
Six weeks after the patient received Invisalign clear aligners, her upper right central incisor appeared purple when intrusion and retraction forces were applied. At this time, clear aligner therapy was suspended and she was referred to an endodontist, according to the report.
The crown of the tooth was a purple color, and the marginal gingival and papilla appeared red and swollen. The tooth didn't respond to cold or heat or electric pulp testing.
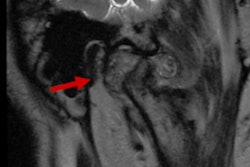
The tooth had mobility and responded to vertical and horizontal percussion. The patient underwent a cone-beam computed tomography scan, which revealed a small area of apical radiolucency on the tooth accompanied by the widening of periodontal ligament space, Zhu wrote.
The clinician suspected transient apical breakdown, therefore endodontic treatment was not initiated, and the tooth was monitored. One month later, the discoloration was less visible, and the gingival inflammation and excessive mobility of the tooth recovered to normal condition.
Additionally, the tooth responded within normal limits to percussion, as well as pulp vitality tests. However, there were no significant radiographic changes, the author wrote.
At the three-month follow-up visit, the woman's tooth had markedly recovered. Her tooth color had improved, and her periodontal status and mobility were normal.
The results of pulp vitality tests were like the last exam, and imaging showed that the small area of apical radiolucency of the tooth remained, but the periodontal ligament space had returned to normal. At this time, it was suggested that she return to her orthodontic treatment, according to the report.
At a six-month visit, the tooth was asymptomatic and returned to its original shade, and the gap between her upper incisors had resolved after the orthodontic treatment, Zhu wrote.
Zhu noted that the report had a limitation, which was that the follow-up time was too short to monitor the status of pulp vitality and tooth color. Follow-up times should be one to two years, the author wrote.
A teaching moment
Transient apical breakdown seems to be a repairing process that occurs in the pulp and periapical areas of traumatized teeth that can sometimes result in crown discoloration.
When discoloration occurs during orthodontic treatment, the first move should be to lighten or remove the orthodontic force. Also, clinicians must consider transient apical breakdown as the potential cause of the crown discoloration, and treatment should be postponed, the author wrote.
"The condition of the discoloured tooth should be monitored with periodic follow-up examinations," Zhu wrote.