Dentists are on the front line in the war against antibiotic-resistant bacteria, said Peter Jacobsen, DDS, PhD, at the recent California Dental Association's CDA Presents 2017 meeting in San Francisco. During his presentation, he provided guidelines for writing safe and effective antibiotic prescriptions for everyday dentistry.
In his well-attended lecture, Dr. Jacobsen outlined what types of antibiotics work best for dentistry and emphasized the importance of measured antibiotic prescribing.
"We're trying to keep our antibiotics as long as possible, and you and I, as part of dentistry, get to be part of that crusade," he said. "Use antibiotics only when indicated -- the right drug at the right dose at the right time."
Dr. Jacobsen is an adjunct professor in the department of pathology and medicine at the University of Pacific Arthur A. Dugoni School of Dentistry in San Francisco.
Types of antibiotics and use cases
Dentists prescribe about 10% of antibiotics in the U.S., according to Dr. Jacobsen. The overwhelming top choice is amoxicillin, which accounts for more than half of all antibiotic prescriptions by dentists. Clindamycin comes in second at 14% of prescriptions, followed by penicillin-VK at 13%.

Amoxicillin and penicillin both work best for the organisms of the oral cavity, Dr. Jacobsen said. Perhaps the most notable difference between the two is that amoxicillin has a longer half-life, so it has to be taken fewer times per day than penicillin. Even one less pill to take can make a big difference for patient compliance, he noted.
"If you take one tablet a day, 73% of people comply," Dr. Jacobsen said. "Three times a day, it's already down to half of patients will comply with that. You have to make clear how these things are going to make them better."
If amoxicillin and penicillin aren't working, Dr. Jacobsen recommended switching to clindamycin, which is more powerful but also has stronger adverse effects, including pseudomembranous ulcerative colitis.
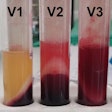
Some specialists will add metronidazole for patients who have had ulcerative colitis. However, metronidazole has a high risk for drug interactions and turns urine a dark brown color, and patients should not drink alcohol while taking it. He recommended consulting with an endocrinologist before prescribing it.
As for patients who get an upset stomach when they take antibiotics, Dr. Jacobsen recommended having them balance antibiotics with probiotics, such as DanActive (Dannon), Florastor (Florastor), and Culturelle (Culturelle Probiotics). He also cautioned dentists to watch out for the bacterium Clostridium difficile with clindamycin and all other antibiotics.
When is antibiotic prophylaxis necessary?
For patients with heart conditions, antibiotic prophylaxis is only recommended for the highest-risk, worst-outcome conditions, Dr. Jacobsen said. These include patients with a prosthetic cardiac valve, a previous history of infective endocarditis (IE), or who have had a heart transplant and developed cardiac valvulopathy.
"Often these patients know they need to be prophylaxed," Dr. Jacobsen said. "They know they might die of their heart problem no matter what."
For these patients, prophylaxis is recommended for all dental procedures and events that involve manipulation of the gingival tissue or the periapical region, but it is not recommended for losing baby teeth, bleeding from trauma to the lips or oral mucosa, and placement or adjustment of orthodontic bands. There is a gray zone, though, for procedures such as biopsies, suture removal, and placement of orthodontic bands when prophylaxis may be reasonable, but its effectiveness is unknown.
If a patient is already taking an antibiotic, Dr. Jacobsen advised selecting a drug from a different class and, if possible, to delay the procedure by 10 days. Also, be alert for infective endocarditis, which presents like the flu with the presence of fever.
"Be suspicious. If it seems like they have the flu, what do they probably have? The flu," he said. "But if your patient is at risk for IE, send them to their physician to rule out something systemic."
As for patients with prosthetic joints, prophylactic antibiotics are generally not recommended before any dental procedures, Dr. Jacobsen said.
"There is no scientific evidence documenting the value of prophylaxing any dental patient to prevent a prosthetic joint infection," he cautioned. "There is scientific evidence documenting side effects and complications from unnecessary antibiotic use. Essentially, not using antibiotics may be safer than using them."
However, a patient's risk for joint infection may be increased if he or she is severely immunocompromised, has poor glycemic control, or has a history of joint infection or a more recent joint replacement. In this case, Dr. Jacobsen recommended consulting the appropriate use criteria online portal from the American Academy of Orthopedic Surgeons, which is a tool designed to "define clinical situations in which antibiotic prophylaxis in certain at-risk dental patients could reduce a theoretical risk of postsurgical prosthetic joint infection," according to the website.
If antibiotic prophylaxis is deemed recommended, Dr. Jacobsen noted that orthopedic surgeons prefer cephalosporin, and the American Heart Association strongly urges against clindamycin.
Finally, if a primary care provider wants his or her patient to take an antibiotic before a procedure, Dr. Jacobsen cooperates but lets the medical provider take charge.
"I'm right behind them," Dr. Jacobsen said. "You write the prescription. I'll do the dentistry."