Ohio dental researchers have found a method to study how T cells cause inflammation during oral candidiasis infections, according to a new study in the Journal of Visualized Experiments (February 18, 2015). The discovery could lead to new therapies or drugs that may improve the functioning of weakened immune systems.
 Pushpa Pandiyan, PhD. Image courtesy of Case Western Reserve University.
Pushpa Pandiyan, PhD. Image courtesy of Case Western Reserve University.Pushpa Pandiyan, PhD, an assistant professor at Case Western Reserve School of Dental Medicine, and colleagues worked on mice to find a new way to model how T cells, the white blood cells critical for the body's immune system, cause inflammation.
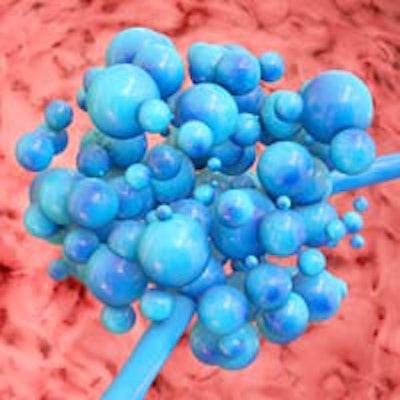
Pandiyan's previous work focused on isolating different types of oral T cells for study. In the latest study, the researchers injected T cells into genetically engineered immunodeficient mice to test how the cells function when fighting Candida albicans, a fungus found in about 60% of the population but controlled by a functioning immune system.
The infection becomes a particular health problem for people with the HIV/AIDS infection, cancer patients with immune systems weakened by chemotherapy, or those born with no immune defenses.
The researchers investigated how IL-17a (T helper 17, or Th17 cells, a type of T cells that secrete a cytokine) and T regulatory cells (Tregs) controlled the fungal infection and inflammation, respectively.
"Although Th17 cells are required for antifungal immunity, uncontrolled Th17 cells have been implicated with such illnesses as multiple sclerosis, lupus, psoriasis, cancers, and irritable bowel disease," Pandiyan said in a statement.
The immunodeficient mice were infected with the fungus and injected with Th17 cells. One group of mice was also injected with Tregs.
The group of mice that received both Th17 and Tregs fared better in stopping the infection and thriving during inflammation, the researchers found. The other group of mice that did not receive Tregs lost weight and began to waste away.
The researchers also found the immune system doesn't work well when the Th17 cells malfunction without appropriate control. "They can set into action a series of immune responses that develop into inflammation and greater health issues," Pandiyan said.
While Pandiyan studied Th17's role in fighting C. albicans, other researchers could use the method to study Th17 cell functions in other areas of the body, she noted.
Pandiyan believes the process could lead to identifying and testing new drugs to replace antifungal medicines that have become ineffective as the fungi develop a resistance to them.